In the past two decades, mind–body interventions (MBIs) have been gaining empirical support and recognition by mental health professionals. Some MBIs, such as Tai Chi, and Qigong, have a strong physical component, others like yoga/meditation and mindfulness, breathregulation techniques, and the relaxation response (RR) are mainly sedentary. Despite the variability in these techniques, they all seem to produce various psychological benefits on healthy and clinical populations, such as the reduction of perceived stress, the alleviation of depression, decreases in anxiety or to help in coping with a chronic medical disease.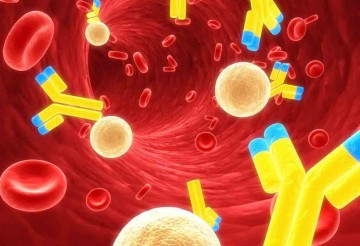
In the context of research on MBIs, the most researched transcription factors are those that have been associated with stress and inflammation. The key transcription factor is the nuclear factor kappa B (NF-κB), which is produced when stress activates the sympathetic nervous system (SNS). NF-κB translates stress into inflammation by changing the expression of genes which code for inflammatory cytokines. Lower activity of NF-κB suggests reduced inflammation.
Stress can be regarded as a bodily response to events that are perceived as a threat or a challenge. This response may precipitate a health risk when stress is severe or it occurs over a long period of time without adequate coping mechanisms. It has been found that exposure to severe stressors can have a profound influence on the body and can lead to detrimental changes in its biology, such as reduced gray matter in several brain regions.
The effects of stress go beyond the brain and can be found in our genes in a form of a CTRA. CTRA is a common molecular pattern that has been found in people exposed to different types of adversities, such bereavement, cancer diagnosis, trauma, and low socioeconomic status. The primary characteristic of CTRA is the upregulation of pro-inflammatory genes leading to major inflammation at the cellular level.
While acute inflammation is a short-lived adaptive response of our body, which increases the activity of the immune system to fight injury or infections, chronic inflammation is maladaptive because it persists when there is no actual threat to the body. Chronic inflammation is associated with increased risk for some types of cancer, neurodegenerative diseases, asthma, arthritis, cardiovascular diseases, and psychiatric disorders (e.g., depression and posttraumatic stress disorder). The secondary characteristic of CTRA is the downregulation of antiviral and antibody-related genes, which is associated with susceptibility to viral infections, such as herpes simplex viruses, HIV-1, Epstein–Barr virus, cytomegalovirus, and the Kaposi’s sarcoma.
The underlying mechanisms are not fully understood. Slavich and Irwin suggested that the environmental stressor, which might be a physical or social threat, will first activate brain regions associated with pain; then, it will project into lower regions that modulate inflammation via the hypothalamus–pituitary–adrenal (HPA) axis and the SNS.
It is likely that CTRA played an important role in our hunter-gatherer prehistory, as it linked fight-or-flight response with pro-inflammatory gene expression that provided protection when there was a higher risk of bacterial infections from wounds. This immune response might have been adaptive back then, but, in today’s modern societies where stress is primarily the result of psychological threats, this response is maladaptive as it promotes inflammation-related diseases, both psychiatric and medical.
Conclusion of 18 studies:
Most studies (81%), that measured the activity of inflammation-related genes and/or NF-κB, a key transcription factor that controls the expression of inflammation-related genes, found a significant downregulation, which can be understood as the reversal of the molecular signature of the effects of chronic stress.
Source: Buric et al. Frontiers in Immunology 2017